Goldilocks Effect and Edema⁚ A Comprehensive Overview
This overview explores the “Goldilocks effect” – the principle of finding the optimal balance – in the context of edema management. Edema‚ fluid buildup in body tissues‚ necessitates a balanced approach. Neither excessive nor insufficient fluid intake is ideal; finding the “just right” amount is key to effective treatment and recovery.
Understanding the Goldilocks Effect
The Goldilocks effect‚ derived from the children’s tale‚ illustrates the preference for optimal conditions—not too much‚ not too little‚ but just right. This principle transcends the fairytale‚ finding application in diverse fields‚ including medicine. In the context of edema‚ the Goldilocks effect highlights the crucial balance required for effective management. For instance‚ hydration plays a vital role; insufficient fluid intake can exacerbate dehydration‚ while excessive intake might worsen edema. Similarly‚ dietary factors and lifestyle modifications need careful consideration to achieve the optimal balance‚ avoiding extremes that could hinder recovery. The Goldilocks effect emphasizes the importance of individualized treatment plans tailored to the patient’s specific needs and circumstances‚ avoiding a one-size-fits-all approach. This nuanced understanding is crucial for successful edema management.
Edema⁚ Causes and Symptoms
Edema‚ characterized by fluid accumulation in body tissues‚ manifests as swelling‚ often in the legs or arms. This swelling can cause skin to appear stretched and shiny‚ sometimes exhibiting pitting—a dimple remaining after pressing the skin. The underlying causes of edema are diverse‚ ranging from relatively benign factors to serious medical conditions. Heart failure‚ for example‚ can impair the heart’s ability to pump blood effectively‚ leading to fluid buildup. Kidney disease can disrupt the body’s fluid balance‚ resulting in edema. Liver disease can similarly contribute to fluid retention. Other factors include lymphatic obstruction‚ venous insufficiency‚ and certain medications. The severity of edema varies‚ ranging from mild swelling to significant fluid retention causing discomfort and functional limitations. Accurate diagnosis requires identifying the root cause‚ enabling targeted treatment strategies. Prompt medical attention is crucial‚ particularly if edema is accompanied by other symptoms‚ to address the underlying condition effectively.
The Goldilocks Effect in Edema Management
The “Goldilocks effect” aptly describes the delicate balance required in edema management. Treatment isn’t about extremes; it’s about finding the optimal approach. For instance‚ hydration is crucial; however‚ excessive fluid intake can worsen edema‚ while insufficient hydration can dehydrate the patient. Similarly‚ medication dosages must be precisely tailored. Too much can lead to adverse effects‚ while too little may prove ineffective. Dietary adjustments‚ such as sodium restriction‚ need careful consideration. Severely limiting sodium can be detrimental‚ while inadequate restriction may impede fluid removal; The Goldilocks principle emphasizes the importance of individualized treatment plans. A healthcare professional assesses each patient’s specific needs‚ considering factors like underlying health conditions‚ lifestyle‚ and response to therapy. This nuanced approach helps ensure the treatment is neither too aggressive nor too passive‚ promoting effective edema reduction while minimizing potential risks.
Fluid Balance and Edema
Edema‚ characterized by excess fluid accumulation in body tissues‚ is intrinsically linked to fluid balance. Maintaining proper fluid balance is essential for preventing and managing edema. This involves a complex interplay of several physiological processes‚ including fluid intake‚ fluid excretion‚ and the distribution of fluids within the body’s compartments. When the balance is disrupted‚ for example‚ due to impaired kidney function or heart failure‚ edema can develop. The body’s inability to effectively eliminate excess fluid leads to its accumulation in interstitial spaces‚ causing swelling. Conversely‚ inadequate fluid intake can lead to dehydration‚ which‚ while not directly causing edema‚ can exacerbate existing conditions and complicate treatment. Understanding the intricate mechanisms governing fluid balance is therefore paramount in managing edema. Effective interventions focus on restoring this balance through appropriate dietary modifications‚ medication‚ and lifestyle adjustments‚ ensuring sufficient fluid intake to prevent dehydration without overwhelming the body’s capacity to eliminate excess fluid.
Optimal Hydration Strategies
Optimal hydration is crucial in managing edema‚ but finding the “Goldilocks” amount—neither too much nor too little—is vital. Overhydration can worsen edema by further stressing the circulatory and lymphatic systems‚ already challenged by fluid retention. Conversely‚ dehydration concentrates the remaining fluid‚ potentially increasing its viscosity and hindering lymphatic drainage‚ thus worsening edema. The ideal hydration strategy involves consistent‚ moderate fluid intake throughout the day. Water is the best choice‚ but other fluids like diluted juices or herbal teas can contribute. Individual fluid needs vary depending on factors like activity level‚ climate‚ and overall health. Monitoring urine output is a helpful indicator⁚ pale yellow urine suggests adequate hydration‚ while dark yellow urine signals potential dehydration; For those with edema‚ consulting a healthcare professional is vital to determine personalized hydration guidelines. They can consider the underlying cause of edema and adjust recommendations accordingly‚ ensuring the hydration strategy supports‚ rather than hinders‚ the overall treatment plan. A balanced approach‚ avoiding both extremes of overhydration and dehydration‚ is key to successful edema management.
The Role of Lymphatic System
The lymphatic system plays a critical role in fluid balance and edema resolution. This network of vessels and nodes collects excess interstitial fluid (fluid surrounding cells) and returns it to the bloodstream. Efficient lymphatic drainage is essential for preventing fluid buildup in tissues. When lymphatic function is compromised‚ either through blockage or impairment‚ fluid accumulates‚ leading to lymphedema‚ a specific type of edema. Factors like infection‚ surgery‚ radiation therapy‚ or genetic predisposition can disrupt lymphatic flow. The lymphatic system also plays a crucial role in the immune response‚ filtering out waste products and pathogens. In edema management‚ supporting lymphatic function is vital. Techniques like manual lymphatic drainage (MLD)‚ a specialized massage technique‚ can help stimulate lymphatic flow and reduce swelling. Compression therapy‚ using bandages or garments‚ also assists by supporting the lymphatic system and preventing further fluid accumulation. Maintaining a healthy lifestyle‚ including regular exercise and a balanced diet‚ indirectly supports lymphatic health. Addressing any underlying lymphatic dysfunction is crucial in effectively managing edema and preventing its recurrence. A holistic approach to treatment often involves improving lymphatic flow.
Treatment Approaches for Edema
Edema treatment strategies are multifaceted and tailored to the underlying cause. For example‚ heart failure-induced edema necessitates managing cardiac function with medications like diuretics to reduce fluid retention. Kidney disease-related edema requires addressing renal function through medication or dialysis. In cases of liver disease‚ managing liver function becomes paramount. Beyond addressing the root cause‚ several approaches directly target fluid reduction. Diuretics‚ medications that increase urine production‚ are frequently used to eliminate excess fluid. Compression therapy‚ involving bandages or specialized garments‚ helps reduce swelling and improve lymphatic drainage. Elevation of the affected limb also aids in fluid reduction. Manual lymphatic drainage‚ a specialized massage technique‚ can stimulate lymphatic flow. In severe cases‚ surgical intervention might be necessary‚ particularly for lymphatic obstruction. The choice of treatment depends heavily on the severity of edema‚ the underlying condition‚ and the individual’s overall health. Regular monitoring of edema and adjustments to treatment are often required. Patient education on lifestyle changes—such as diet and activity—is also integral to long-term edema management and overall well-being.
Dietary Considerations for Edema
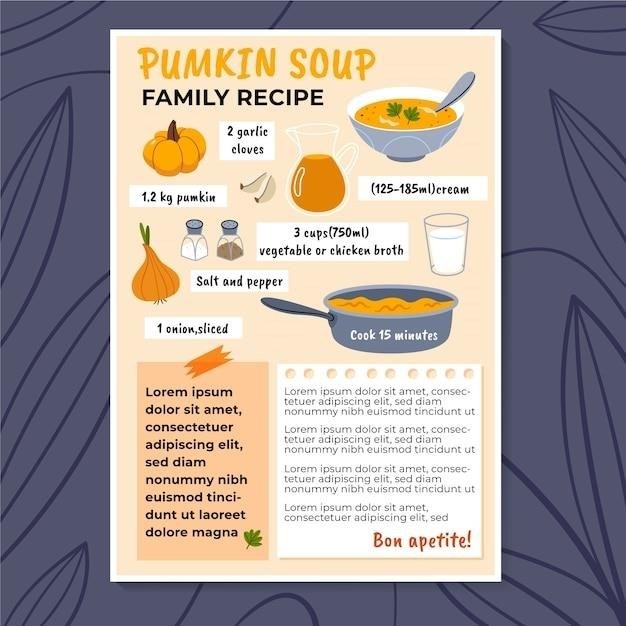
Dietary modifications play a crucial role in edema management‚ focusing on fluid balance and reducing sodium intake. Excessive sodium consumption leads to water retention‚ exacerbating edema. Therefore‚ a low-sodium diet is vital. This involves limiting processed foods‚ canned goods‚ and salty snacks. Fresh fruits‚ vegetables‚ and whole grains are encouraged‚ as they are naturally low in sodium. Additionally‚ monitoring fluid intake is crucial. While adequate hydration is essential‚ excessive fluid intake can worsen edema. Finding the optimal balance—the “Goldilocks” amount—is key. The dietary approach should also consider the underlying cause of the edema. For example‚ individuals with liver disease may need to restrict potassium intake‚ while those with kidney disease may need to limit protein or phosphorus. Consulting a registered dietitian or nutritionist specializing in edema management is recommended to create a personalized dietary plan that addresses individual needs and health conditions. The dietitian can help develop a meal plan that balances nutritional needs while managing fluid and sodium intake effectively. This personalized approach ensures optimal support for edema reduction and overall health improvement.

Lifestyle Modifications for Edema Reduction
Beyond diet‚ lifestyle adjustments significantly impact edema management. Regular exercise‚ particularly low-impact activities like walking or swimming‚ promotes lymphatic drainage and reduces fluid retention. However‚ excessive exertion should be avoided‚ as it can strain the circulatory system. Finding the right balance—the “Goldilocks” level of physical activity—is crucial. Elevation of the affected limbs also aids in reducing edema. Elevating legs when resting helps fluid flow back towards the heart‚ reducing swelling in the lower extremities. Maintaining a healthy weight is essential‚ as excess weight puts added strain on the circulatory and lymphatic systems. This can worsen edema‚ especially in the legs and ankles. Furthermore‚ smoking cessation is vital‚ as smoking damages blood vessels‚ potentially worsening fluid retention and edema. Finally‚ stress management techniques like yoga‚ meditation‚ or deep breathing exercises are beneficial. Chronic stress can negatively impact circulatory function‚ contributing to fluid retention. Implementing these lifestyle changes‚ in conjunction with dietary adjustments and medical treatment‚ creates a comprehensive approach to edema reduction‚ emphasizing a balanced and sustainable lifestyle for long-term health improvement.
Case Studies and Research
While a specific “Goldilocks effect edema recipe PDF” doesn’t exist in readily available research‚ numerous studies highlight the importance of balanced interventions. Research on edema management frequently emphasizes the need for individualized treatment plans. A patient’s response to therapy varies significantly‚ requiring careful monitoring and adjustments to achieve optimal results. Case studies often illustrate the effectiveness of combining dietary changes‚ medication‚ and lifestyle modifications. For instance‚ a study might detail a patient with heart failure-related edema whose symptoms improved significantly after implementing a low-sodium diet‚ taking diuretics‚ and increasing physical activity‚ demonstrating the synergistic effect of a multi-faceted approach. Other research focuses on specific edema types‚ such as lymphedema‚ exploring the efficacy of manual lymphatic drainage‚ compression therapy‚ or exercise programs. The collective evidence suggests that a balanced strategy‚ adapting treatments to individual needs and responses‚ mirrors the “Goldilocks” principle⁚ not too much‚ not too little‚ but just the right intervention for optimal edema reduction. Further research is needed to refine personalized treatment protocols‚ incorporating individual factors like age‚ overall health‚ and the underlying cause of edema for better outcomes.
Conclusion and Future Directions
In conclusion‚ while a single “Goldilocks effect edema recipe PDF” is not a scientifically validated concept‚ the underlying principle of achieving optimal balance in treatment is paramount. Managing edema effectively requires a personalized approach‚ considering individual factors and tailoring interventions accordingly. Future research should focus on developing more precise diagnostic tools and predictive models to better identify patients at risk for edema and to individualize treatment plans. This includes exploring the role of advanced imaging techniques to better visualize fluid accumulation and the lymphatic system’s response to therapy. Furthermore‚ investigations into novel therapeutic strategies‚ such as targeted drug delivery systems and advanced compression technologies‚ are warranted. A deeper understanding of the complex interplay between fluid dynamics‚ lymphatic function‚ and the underlying disease processes is crucial. By integrating these advancements‚ clinicians can move towards a more precise and effective approach to edema management‚ truly embodying the “Goldilocks” principle of finding the just-right balance for each patient to achieve optimal outcomes and improve their quality of life.